| ||
| ||
╠¤ |
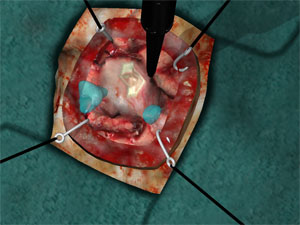
This innovative neurosurgical simulator signals a significant leap forward in patient care and safety, allowing doctors to rehearse complex surgeries long before a patient enters the surgical suite. The realistic and elaborate simulation was constructed using the patientтАЩs own detailed brain imaging studies performed in Halifax.
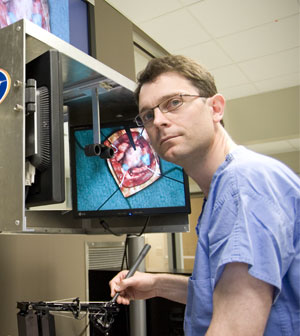
тАЬThe simulator enabled us to map out and perform our surgical plan in virtual reality prior to the actual surgery,тАЭ said Dr. David Clarke, professor of neurosurgery at ║┌┴╧│╘╣╧═ЇMedical School, staff neurosurgeon at Capital Health, member of the Brain Repair Centre, and collaborator in the National Research Council (NRC) project. тАЬThis means we are able to do a dry-run of the surgery to better determine how to remove the tumour safely.тАЭ
The neurosurgical team took pictures of the patientтАЩs brain using an MRI at the Queen Elizabeth II Health Sciences Centre. Then using the virtual reality neurosurgical simulator developed by researchers at the NRC, Dr. Clarke mapped out the tumour and his subsequent surgical approach.
Brain tumour surgery is high risk because of potential damage to surrounding brain tissue and possibility of tumour recurrence. For these reasons, procedures are becoming less invasive, yet more complex, and therefore require extensive training to ensure patient safety. The simulator will be used for both benign and malignant tumours.
 |
| The surgical team and patient in the operating theatre. |
тАЬThis technology will make brain surgeries safer for patients, and will be used to train the next generation of surgeons at ║┌┴╧│╘╣╧═ЇMedical School,тАЭ says Dr. Ryan DтАЩArcy of the National Research Council and ║┌┴╧│╘╣╧═Ї. тАЬInnovative health care solutions, such as the virtual reality neurosurgery simulator, enable us to deliver top-quality medical care to Canadians.тАЭ
The neurosurgical simulator project involves a cross-Canada collaboration of high-profile and nationally renowned clinical collaborators and research scientists in Vancouver, Calgary, Winnipeg, Toronto, Montreal and Halifax. NRC is preparing to transfer seven prototypes of the neurosurgical simulator to Canadian hospitals over the next two years.
тАЬThis simulator will become a key component of neurosurgical training and will help to optimize patient outcomes and recovery,тАЭ says Dr. Clarke. тАЬBy practising surgeries in advance of the real thing, weтАЩll be better able to anticipate and fix potential problems before they occur. Brain tumour patients in Canada will have access to the best, most advanced care in the world.тАЭ
IN THE NEWS: on CBC | from Canadian Press